Treatments
Here you will find just a small sampling of the range of resources Abbotsford Physiotherapy can bring to bear on a small selection of the ailments we treat.
Depending on the results of the assessment of your ailment performed on your first visit to us, your specific treatment regime may differ from the samples outlined here. Remember, an initial assessment of your ailment is as close as the phone.
To make an appointment please phone (604) 855-5157.

Treatment
Pain releif with anti-inflammatory modilities such as laser, ultrasound & interferential or micro currents.
Range of Motion Maintenance
Manual Therapy, Exercise
Strengthening
Muscle stimulation with specific exercises, gym exercises
Management
Home exercise program; posture & positioning; advise on bracing, orthotics & home pain relief
Concussion Injuries

Spinal Assessment
Checking all areas of the spine for alignment and spinal subluxations.
Strength Training
Specific spinal stabilization exercises to improve strength around injured vertebrae joints
Stretching Exercises
Soft tissue stretching around injured areas.
Activity Education
Symptom management during progressive activity to allow a safe return to activities.

Pain Relief
Ice, heat, whirlpool, anti-inflammatory modalities, electro-magnetic field therapy.
Range of Motion
Manual therapy, progressive exercises
Strength Training
Biofeedback, muscle stimulation, gym exercises.
Gait Training
Gait analysis and correction to allow for efficient movement pattern
Management
Home exercise regime, return to function advice

Treatment
Manual / Manipulative Therapy to correct the faulty spinal/pelvic position creating the pain.
Pain Control
Through the use of modalities like Ultrasound, Laser, and Interferential currents.
Strengthening
Spinal/Core stabilization exercises to prevent future subluxations.
Management
Home exercises and education on ice/heat.

Pain & Inflammation Relief
Ice, Heat or Whirlpool, Ultrasound, Laser, Interferential or Mirco Current, Traction
Restoration of Mobility
Progressive Range of Motion exercises, manual therapy
Restoration of Strength
Biofeedback, muscle stimulation, graduated strengthening exercises, gym program
Management
Sport/Work modification, taping/bracing, posture corrections, home exercise program

We are excited to be offering pelvic health physiotherapy. Physiotherapist Alysha Sieben has taken specialized training in pelvic floor rehabilitation. She is a mom herself and is passionate about helping women live healthy and active lifestyles.
A pelvic health physiotherapist can help with many conditions including but not limited to:
- Pelvic pain (pubic symphysis, Sacroiliac (SI) joint, & tail bone pain)
- Prenatal and postnatal care
- Pelvic organ prolapse
- Pain during intercourse
- Bladder and bowel conditions (incontinence, urgency, constipation)
- Menopause
- Other conditions: painful periods, interstitial cystitis, endometriosis, post-operative pelvic surgeries, vaginal dryness, persistent low back pain and more.
If you do not see the condition listed above please call our clinic at 604-855-5157 or email [email protected] to discuss any concerns and if pelvic floor physiotherapy can help you.
Pregnancy Care:
A pelvic floor physiotherapist can provide you with tools and strategies to make you feel more confident when going through pregnancy and delivery. During your treatments, the therapist will assess how your pelvic floor functions and teach you how to contract and relax your pelvic floor. You will be provided with information on safe exercise during pregnancy. A pelvic health physiotherapist can also help alleviate pain experienced throughout your pregnancy.
Postpartum Care:
Women can benefit from seeing a pelvic floor physiotherapist anytime after 6 weeks postpartum especially those with a grade 2 or higher perineal tear. A pelvic health physiotherapist can provide you with information and tools to help assist in your recovery.
Pelvic Organ Prolapse
A pelvic organ prolapse is often accompanied by a feeling of heaviness in the pelvic region or vagina. It is common after labor and delivery and can be accompanied by pelvic pain, incontinence, and weakness. During your initial assessment, you will be assessed for a pelvic organ prolapse during an internal exam (if you consent and are comfortable) and treatment will be provided as needed.
Diastasis Recti Abdominis:
In order to accommodate for a growing baby the rectus abdominis muscle commonly known as the “six pack muscle” separates from the soft tissue that holds it together called the lina alba. This is a normal process to allow for the growth of your baby. Sometimes this muscle remains in this changed position and is called “diastasis recti abdominis”. A diastasis recti abdominis may be accompanied by a feeling of weakness in your stomach or core. Our therapist can provide you with stability and mobility exercises to strengthen this area.
Incontinence:
Urinary incontinence or the involuntary loss of urine is a common report by women. 20-30% of younger women and 30-40% of middle age women report urinary incontinence (Eliasson et al., 2005). Stress incontinence happens when the pelvic floor is placed under physical strain such as coughing, sneezing, laughing, or exercising. Urgency incontinence is the loss of urine with urgency. Incontinence is preventable and not normal.
Eliasson, K., Elfving, B., Nordgren, B., & Matteson, E. (2006) Urinary incontinence in women with low back pain. Manual Therapy, 13. (2008), 206-212
Recovery from cesarean section ( C-section)
A cesarean section is a major abdominal surgery. It takes time for your body to recover especially when you are caring for a baby! Women who undergo cesarean sections often report musculoskeletal pain, pelvic pain, weakness, and burning in and around their scar. A pelvic health physiotherapist can help you prepare for a planned cesarean and manage your symptoms afterwards. Treatment often consists of scar management, breathing exercises and strengthening your core and pelvic floor. Our therapist can show you positions to decrease tension and pain on your scar while breastfeeding your baby.
Returning to exercise
After having a baby your body needs time to heal. A pelvic health Physiotherapy will educate you on what exercises to avoid doing and provide you with exercises that are tailored to where you are in your recovery. Our therapist can assess and provide you with information on when it is safe to return to higher impact activities like running.
Breastfeeding and carrying your baby:
A pelvic floor physiotherapist can assess your posture and recommend positions that may make it easier on your body while breastfeeding, bottle feeding, or carrying your baby. Breast feeding may be accompanied by neck, mid back and shoulder pain. Certain postures may also cause discomfort in a cesarean scar while it is healing. Our therapist uses manual therapy, exercise, education on posture, and more to make it easier on you to continue breastfeeding.
Pain with intercourse:
Pain associated with intercourse is reported by women who have had babies and by women that have not had babies. A pelvic floor therapist can help to determine what may be the cause of your pain and help to decrease your pain. Sex does not have to be painful!
Perimenopause/ Menopause/ Postmenopause
Menopause is caused by a change in the hormones estrogen and progesterone which can affect the way your body absorbs forces and recovers from activity. A pelvic floor therapist can help you through this transition.
Post Mastectomy/ lumpectomy:
Physiotherapy can help with scar management, improving range of motion and strength in the joints and muscles around the chest and rib cage including the neck, mid back, and shoulder. Our therapist can provide you with guidance on returning to your activities and lifestyle after surgery.
Osteoporosis:
Osteoporosis is common in females and risk increases after menopause. All of our health care providers can help to assess and treat stiffness, pain, or weakness associated with osteoporosis. Treatment consists of providing you with information and tools to help manage your symptoms, strengthening and mobility exercises, advice on exercise, and an exercise program tailored to meet your goals.
What does pelvic floor physiotherapy assessment and treatment consist of?
During your first visit you will be asked for a detailed health history about your area of concern, gynaecology and obstetrics history, lifestyle history, overall health, and any other present or past injuries or illnesses. You will be educated on your pelvic health concern and may be provided with resources and information to give you more knowledge about the area.
You can expect a combination of the following assessment and treatment techniques:
- Manual hands-on therapy in the pelvic region including joint mobilization & soft tissue release
- Postural assessment
- Walking & running assessment
- Strengthening exercises
- Intramuscular stimulation (IMS)
- Diaphragm & breathing exercises
- Relaxation exercises
- Mobility and stretching exercises
- Therapeutic modalities (LASER, shockwave, TENS/ IFC, therapeutic ultrasound)
- Internal vaginal and/ or rectal exam (with your consent and comfort). An internal exam allows the physiotherapist to assess the ability of the pelvic floor muscles to contract and relax. Many women are not doing a pelvic floor contraction properly. During your treatments you will be taught the most efficient way to breath and do a pelvic floor contraction. An internal assessment can also determine if the pelvic floor is referring pain to other areas of the body.

Supersensitivity and muscle shortening cannot be operated on and ‘cut away,’ while ‘painkillers’ and other analgesic pills only mask the pain (often poorly) and promote toxicity, compounding the problem. Neuropathy only responds to a physical input of energy.
Intramuscular Stimulation (IMS) is a total system for the diagnosis and treatment of myofascial pain syndromes (chronic pain conditions that occur in the musculoskeletal system when there is no obvious sign of injury or inflammation). IMS is grounded in Western Medical Science, and has a solid foundation in its radiculopathic model of pain, which is now supported by many experts in the field. It was developed by Dr. Gunn while he was a physician at the Worker’s Compensation Board of British Columbia in the 70′s, where he investigated the large number of mysteriously stubborn cases after frustration with the ineffective modalities at his disposal. The treatment, which utilizes acupuncture needles because they are the thinnest implements available that are designed to penetrate deep within muscle tissue, specifically targets injured muscles that have contracted and become shortened from distress.
IMS relies heavily on a thorough physical examination of the patient by a competent practitioner, trained to recognize the physical signs of neuropathic pain. This physical examination is indispensable since chronic pain is often neurological as opposed to structural, and therefore, invisible to expensive X-rays, MRI Tests, Bone and CT Scans. Failure to recognize these signs will result in an inaccurate diagnosis, and thus, a poor starting point for physical therapy.
The treatment involves dry needling of affected areas of the body without injecting any substance. The needle sites can be at the epicenter of taut, tender muscle bands, or they can be near the spine where the nerve root may have become irritated and supersensitive. Penetration of a normal muscle is painless; however, a shortened, supersensitive muscle will ‘grasp’ the needle in what can be described as a cramping sensation. The result is threefold. One, a stretch receptor in the muscle is stimulated, producing a reflex relaxation (lengthening). Two, the needle also causes a small injury that draws blood to the area, initiating the natural healing process. Three, the treatment creates an electrical potential in the muscle to make the nerve function normally again. The needle used in IMS, by stimulating muscle spindles, essentially becomes a specific and unique tool for the diagnosis of Neuropathic Muscle Pain.
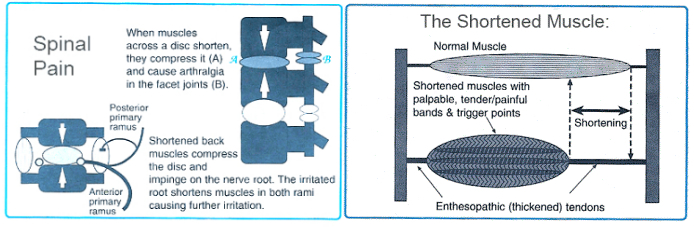
The goal of treatment is to release muscle shortening, which presses on and irritates the nerve. Supersensitive areas can be desensitized, and the persistent pull of shortened muscles can be released. IMS is very effective for releasing shortened muscles under contracture, thereby causing mechanical pain from muscle pull. IMS, in effect, treats the underlying neuropathic condition that causes the pain. When competently performed, IMS has a remarkable success rate, as proven by the amelioration of symptoms and signs, even for chronic back pain with root signs.
IMS is comparable in some ways to acupuncture; however, there are a number of important differences. IMS requires a medical examination and diagnosis by a practitioner knowledgeable in anatomy, needles insertions are indicated by physical signs and not according to predefined, non-scientific meridians, while subjective and objective effects are usually experienced immediately.

What Is Radial Shockwave Therapy?
Shockwave therapy is a safe and non-invasive procedure that applies a series of acoustic wave pulsations directly to the site of injury / dysfunction through the client’s skin via a gel medium. The shockwaves stimulate the body’s natural self-healing process and has been research proven to help treat chronic conditions of the tendons, muscles and joints.
How Does Radial Shockwave Therapy Work?
Shockwave therapy involves a series of intense short physical waves that causes break down of targeted damaged/scared tissue and increased blood flow to that tissue. The body’s response to these physical waves is an increase in the production of new healthy tissue. By creating blood flow and controlled inflammation, it gives the damaged/scared tissue another chance at tissue repair and recovery. Some conditions have a difficult time healing due to the development of unhealthy, disorganized tissue in the injury area. Over time, the body is unable to adequately repair and heal itself. Research has shown shockwave therapy to be highly effective in treating tendon, muscle and joint conditions by stimulating the body’s own natural healing response.
How Long Does Each Treatment Last?
Initially, you will have a thorough assessment by one of our registered physiotherapists to determine if shockwave therapy is an appropriate therapy for your injury or condition. The actual treatment time spent receiving the shockwave therapy is typically less than 5 minutes. Treatments will also include education and an appropriate post-treatment plan.
Is Shockwave Therapy Right For Me?
Shockwave therapy has been scientifically proven to help with:
- Plantar fasciitis
- Achilles tendonitis/tendinosis
- Jumper’s knee / Knee tendonitis/tendinosis
- Calcific tendonitis
- Bursitis
- Trigger points
- Tennis elbow / lateral epicondylitis
- Hallux Rigidus / Big toe stiffness
- Adductor strain
- Hamstring strain
- Calf strain
The success rate has ranged from 70% to 91% improvement, with low complications from treatment (Journal of Orthopaedic Surgery and Research, 2012). Shockwave therapy is a non-surgical option with results that should be considered when other treatment options have failed or the condition continues to return.
How Many Treatment Will I Need?
The research backed protocols outline that most conditions will require 3-5 sessions of shockwave therapy. An additional 2 sessions may be required if the condition is very chronic. Shockwave Canada states that muscular trigger points may require only 1-3 treatment sessions.
Does the Treatment Hurt?
Treatment can be uncomfortable, but it is usually well tolerated. It is an intense 5 minutes that most people can tolerate. Many clients experience a decrease or complete absence of pain immediately after treatment. On rare occasions, bruising and swelling may occur.
Will It Hurt After the Treatment?
There may be some soreness or throbbing 1-2 hours after the treatment session due to an inflammatory response of the body to the shockwave pulses. This is a NORMAL response to treatment and is your body’s way of healing itself and regenerating the targeted tissue. This discomfort usually subsides after 1-2 days.
What Should I DO If I Am in Pain Following the Treatment?
The shockwave will trigger an inflammatory response, which is the body’s natural process of healing. This is the natural process that we are trying to stimulate. Therefore, it is important to try and refrain from using anti-inflammatory medications or ice. Using heat on the treated area can assist in blood flow to the healing tissue.
What If It Feels Good Following the Treatment?
Even if it feels good, we recommend the decreased activity for 48 hours following the treatment.
Is Shockwave Therapy Covered by My Medical Insurance?
You will be invoiced under physiotherapy. If you have physiotherapy benefits it will be covered but check with your provider to be sure.
Precautions / Contra-indications to Radial Shockwave
It is important that you discuss your relevant medical and injury history with your therapist. You may not qualify for radial shockwave therapy, or an individually determined level of caution may have to be practiced if you have any of the following:
- Cortisone injection within the last 6 weeks.
- Bleeding disorder (Clotting conditions, haemophilia, etc..).
- Blood thinning medications/anticoagulant therapy (Heparin, Warfarin, Coumadin).
- Heart or circulatory problems (eg. Pacemaker).
- Cancer / local malignancy.
- Diabetes.
- Pregnancy.
- Blood or nerve supplies too close to the affected area.
- Local nerve tingling or numbness.
- Open wound over the site to be treated.
- Poorly localized or non-palpable area of pain.
- Inflammation or infection at the site of treatment (signs include redness, swelling, fever, etc.).
- Cognitive difficulties (unable to follow directions; Alzheimer’s disease, dementia, brain injury).
At Abbotsford Sports & Orthopaedic Physiotherapy our goal is to help children move with ease and live a pain free active life.
PHYSIOTHERAPY FOR INFANTS:

Areas of treatment include but are not limited to:
Delayed motor milestones:
- Your baby may benefit from physiotherapy if you notice they are rolling, crawling, pulling to stand, standing, walking, jumping, or running later than their peers.
- Our physiotherapists can show you exercises to help your child reach their age appropriate motor milestone.
Torticollis
- Torticollis is when a muscle in the neck called the “sternoceloidmasteoid” (SCM) shortens or becomes “tight”. You may notice your baby holds their head tilted to one side or that they prefer to look, feed, or roll in one direction.
- Torticollis can happen while a baby is in utero, during birth, or after birth.
- Our physiotherapists can show you positions, stretches, and strengthening exercises to help with torticollis.
Plagiocephaly or “ flattening of the skull”
- Infants have a soft skull compared to adults and can sometimes have flattening on the front, side or back of their skulls.
- This condition is important to address when your baby is an infant.
- Torticollis can increase the chances of your baby developing plagiocephaly.
Physiotherapy treatment can include:
- Education – Including prevention and treatment of any of concerns, motor milestone timelines, how to increase tummy time and encourage mobility. Our goal is to educate caregivers so they feel comfortable implementing physiotherapy exercises into everyday life.
- Exercises – tummy time, stretching ,and strengthening exercises, and activities to encourage mobility.
PHYSIOTHERAPY FOR TODDLERS, CHILDREN AND TEENAGERS:

Areas of treatment include but are not limited to:
Pain
Our physiotherapists can assess and treat both acute (sudden) or chronic (long term) pain that may be caused by:
- Ligament sprain or muscle strain
- Bone injury or fracture
- Surgical recovery
- Growing pain or achey muscles/ limbs while sleeping
- Our physiotherapists can assess strength and flexibility and provide exercises that may help alleviate growing pains.
Decreased coordination and/ or balance
Muscle tightness or weakness
Sports injuries
Concussion
Delayed physical milestones or developmental delays
Toe walking, flat feet or any concerns with gait/walking
Growth concerns and childhood injuries (including but not limited to:)
- Sever’s Disease
This is experienced as heel pain when the growth pate at the back of the heel becomes inflamed due to repetitive stress on the Achilles tendon. - Osgood-Schlatter Disease
This is common in activities that require running and jumping. It presents as pain at the front of the knee due to inflammation and irritation of the growth plate at the top of the shin bone. - Jumper’s Knee
This is common in activities that require jumping or stopping and/ or switching directions at high speed. Jumper’s knee is an overuse injury of the patellar tendon that connects your knee cap (patella) to your lower leg bone (tibia) and can result in pain below the knee cap. - Hip Apophysitis
This is caused by a growth plate irritation at the hip from overuse due to repetitive pulling on the muscles that connect to the hip bone. This is common in running athletes (including soccer, rugby, football, track & field athletes), dancers, and gymnasts. Hip Apophysitis typically presents as a dull pain at the front of the hip. - Juvenile idiopathic arthritis (JIA)
What you and your child can expect on your first visit:
Our physiotherapist will ask the child and/or caregiver questions regarding their mobility, pain, and/or concern. This includes questions regarding your child’s health history.
They will then conduct an in-depth assessment to look at how your child moves. This may include:
- Walking/ gait assessment
- Posture assessment
- Strength, flexibility, and range of motion assessment
- Balance & coordination assessment
- Sport specific skills and physical form assessment
- Hands on assessment
Please ensure your child is wearing comfortable clothing that they can move in.
Feel free to bring any of your child’s favourite toys.
A physiotherapy treatment plan will be unique to each child and may include:
- Exercise / rehabilitation program – strengthening, flexibility, balance, and coordination exercises.
- Hands on treatment – soft tissue release of muscles, taping, passive or active stretching, and/or joint mobilizations
- Education – addressing any concerns, sharing knowledge on posture, exercise and/or sport specific training, information on milestone timelines, injury recovery and rehabilitation.
- Modalities – our clinic offers electrical therapy (TENS & IFC), LASER, Shockwave when needed.
Please call our office at 604-855-5157 to book or you have any questions about paediatric physiotherapy.
You can also email [email protected] with any questions.





